In modern healthcare organizations, managing clinical, administrative, and operational risks is an increasingly critical priority. However, risk analysis often remains confined to documents and formal procedures—a “paper exercise” with little impact on day-to-day operations. This happens because reducing the probability of a risk requires continuous monitoring (a time-consuming, cognitively demanding task for staff), while mitigating its impact demands interpreting and evaluating a vast array of precursor data and risk signals in real time. In practice, risk analysis often becomes disconnected from daily work, performed in periodic meetings or retrospective reports rather than integrated into continuous operational activity.
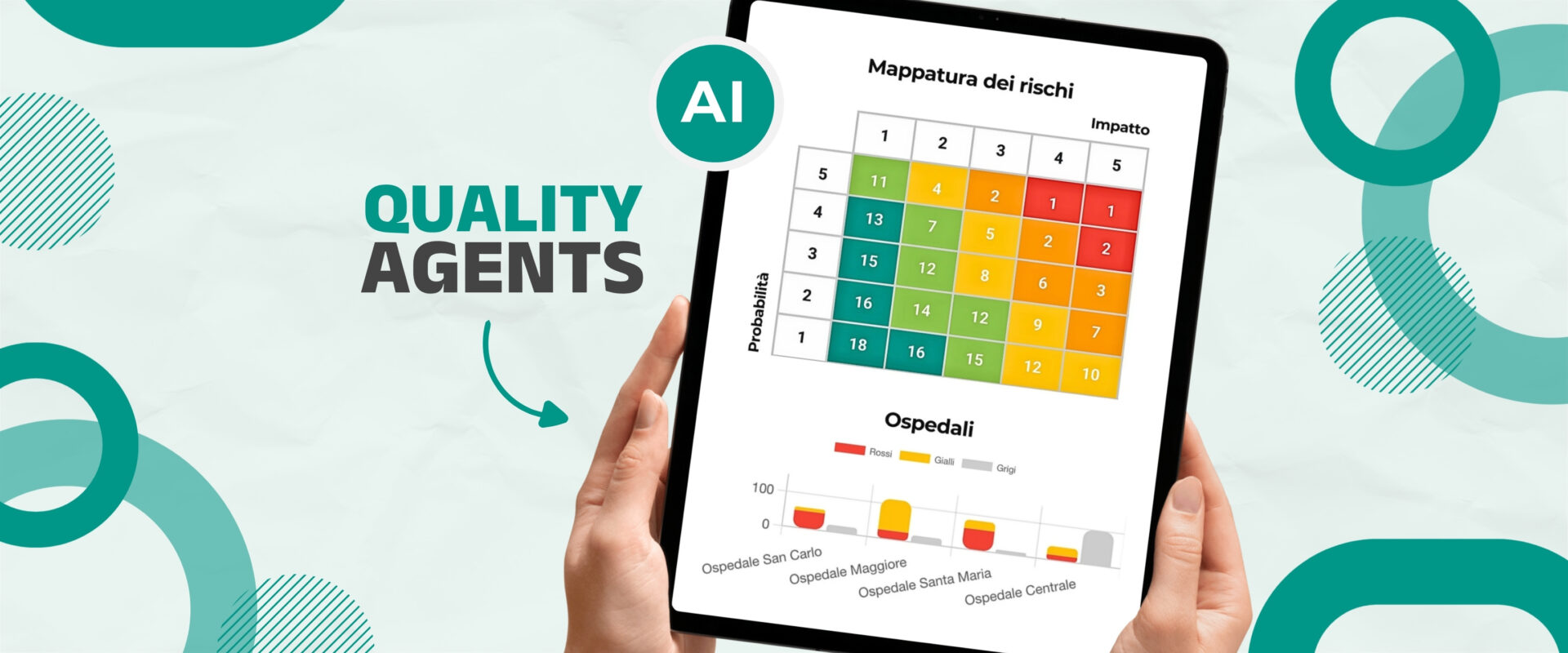
A new approach is changing this scenario: the use of intelligent AI-based agents, known as Quality Agents, operating 24/7. These software agents, tailored to the organization’s data, analyze enormous streams of clinical, administrative, and operational information in real time. Their task is to detect weak signals and anomalies that may indicate potential risks, immediately alerting human staff to areas needing attention. Risk management stops being a post-event theoretical exercise and becomes a proactive, operationally embedded tool: risks are no longer hidden in records or monthly statistics but are brought to light and addressed as they emerge. This shifts the approach from reactive (“acting after an adverse event”) to predictive, where AI helps anticipate adverse events and prevent inefficiencies before they occur.
The tangible benefits are widespread: greater patient safety, improved regulatory compliance, optimized resource use, and reduced unexpected costs due to preventable emergencies.
For risk managers and quality officers, this means having a real-time overview of hundreds of relevant organizational requirements, guiding continuous improvement instead of chasing problems after the fact.
1. Clinical Risk Mitigation: AI Anticipates Adverse Events
The first application area is clinical risk, focused on patient safety and preventing adverse events. Many dangerous situations in hospital wards can be avoided if identified early, but this requires constant surveillance and the ability to detect non-obvious correlations among clinical parameters. An AI “clinical” agent can perform this task continuously across all patient admissions, analyzing electronic health record data to ensure compliance with guidelines and care protocols (PDTAs).
For example, routine steps might occasionally be skipped: an incomplete surgical checklist, an unassessed fall risk, or an abnormal drug dosage not flagged. An AI agent can continuously check all clinical documentation and alert staff immediately if a critical checklist item is missing or a patient assessment is incomplete. Ensuring consistent application of safety protocols reduces the probability of adverse events significantly—e.g., systematic use of the WHO surgical checklist can reduce complications and operative mortality by over 30%. The AI ensures that each team follows protocols correctly, potentially saving lives and preventing serious errors.
2. Compliance and Administration: The Tireless Intelligent Agent
The second example concerns administrative and regulatory risk, where the volume of details and deadlines often exceeds human capacity. Maintaining compliance with laws, accreditation standards, administrative obligations, and documentation is demanding and error-prone: a missing form, overdue equipment maintenance, or ignored regulation can expose the organization to fines or financial losses. A Quality Agent trained on administrative processes acts as an infallible overseer, ensuring nothing “falls through the cracks.”
Scenario: a hospital must ensure all mandatory clinical documentation is present and up-to-date (informed consents, pain assessment scales, treatment plans) while monitoring deadlines such as biomedical equipment calibration, staff mandatory training, insurance renewals, and quality certifications. An AI agent can daily cross-check all databases—from EHR systems to maintenance logs—alerting staff immediately if any document is missing or any deadline is approaching. This drastically reduces the risk of non-compliance and eliminates last-minute stress.
An important benefit is that AI frees human staff from repetitive, cognitively demanding tasks. The machine executes thousands of background checks and flags anomalies instantly, reducing both the likelihood and impact of administrative risks and improving overall organizational quality.
3. Operational Processes and Resources: Preventing Bottlenecks and Crises
The third area, operational risk, relates to workload overloads, inefficiencies, waste, or shortages of staff and equipment—situations that can lead to patient dissatisfaction and avoidable costs. Key to prevention is detecting early warning signals. Operational Quality Agents continuously monitor key performance indicators to identify emerging trends or bottlenecks.
Example: the AI system analyzes real-time data such as bed occupancy per ward, ER waiting times, patient-to-nurse ratios, OR utilization, and critical medical supply levels. If an indicator exceeds thresholds (e.g., ER boarding time surpassing 6 hours while staff shortages occur), the agent immediately alerts management, allowing interventions before situations escalate—calling in additional staff, opening extra beds, or redirecting ambulances.
Monitoring also identifies inefficiencies and resource underuse. For instance, if an OR is used only 50% of the time or expensive diagnostic equipment sits idle, AI highlights these as opportunities for improvement. Adjusting schedules or consolidating procedures increases utilization, reduces surgical waitlists, and maximizes ROI. Likewise, persistently high occupancy rates signal a risk, as studies show chronically overcrowded hospitals see higher patient mortality. Early alerts allow proactive measures, maintaining quality of care.
Towards 24/7 Data-Driven Risk Management
The examples demonstrate how tailored AI agents can make risk management continuous and fully integrated into daily operations. The value goes beyond automating checks or relieving staff of repetitive tasks—it changes the philosophy from reacting after problems occur to preventing them before they happen. Continuous monitoring reduces the likelihood of important signals being missed, even during high-pressure periods.
For healthcare executives and department heads, these systems mean fewer surprises and greater transparency: latent clinical, administrative, or operational risks are detected early and mitigated before escalating into legal disputes, fines, or reputational damage. Economically and strategically, investing in AI for risk management pays off: preventing a major adverse event or systemic inefficiency avoids unexpected costs far exceeding implementation expenses. Hospitals adopting digital monitoring demonstrate commitment to quality and safety, building trust with patients, regulators, and partners.
Finally, AI agents augment, not replace, human staff. They highlight risks early, leaving professionals to assess, decide, and act. This synergy creates a virtuous cycle of continuous improvement, where AI and human expertise combine to build safer, more efficient, and risk-aware healthcare systems.
At Connect, we strongly believe in this innovative approach and are developing expert agents to support clinical, administrative, and operational staff, reducing cognitive load and burnout.
We are available to analyze, with no obligation, difficult cases submitted by healthcare organizations of any type—IRCCS, hospitals, rehabilitation centers, nursing homes, and polyclinic networks. We study the submitted “challenging case,” propose a tailored solution, and provide a feasibility study, all without commitment from the organization.
Contact us to learn how our AI-based Quality Agents can transform risk analysis into actionable, everyday improvements.